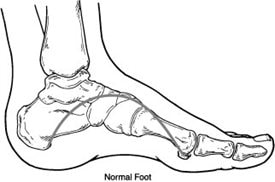
Charcot foot is a serious condition that can affect those with diabetes and peripheral neuropathy, where the bones in the feet weaken, fracture and dislocate.
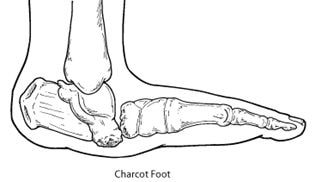 One of the big dangers of the charcot foot process is that it is often painless and devoid of alarming symptoms, particularly in the early (acute) stages, where only a dull ache may be felt that can be easily ignored. Despite this, the changes occurring are serious, with the joints and foot structure ultimately collapsing and leading to a rocker-bottom foot that can present a myriad of complications when it comes to walking and managing daily life.
One of the big dangers of the charcot foot process is that it is often painless and devoid of alarming symptoms, particularly in the early (acute) stages, where only a dull ache may be felt that can be easily ignored. Despite this, the changes occurring are serious, with the joints and foot structure ultimately collapsing and leading to a rocker-bottom foot that can present a myriad of complications when it comes to walking and managing daily life.
While certain symptoms like warmth, redness and swelling may be present, the reduced ability to detect any pain (resulting from having neuropathy) means that many people do not know that there is a problem, or that they should check their feet or see a podiatrist. Neuropathy and nerve damage are also thought to be the cause of charcot foot.
Can you fix it?
While we cannot reverse the damage that has already occurred, we can help prevent or reduce the impact of further damage to help keep you as mobile and comfortable as possible – which makes a world of difference to many patients. Our podiatrists will:
- Confirm your diagnosis, referring you for medical imaging
- Ensure you understand exactly what is happening and why
- Teach you what you should be doing and checking at home every day, so you can detect any ‘warning signs’ both now and in the future
- Help you manage any other consequences of diabetes and neuropathy on your feet
- Form a customised treatment plan, and refer you to other specialists as needed
- Keep you fully supported throughout the process
How is a Charcot foot treated?
After your diagnosis has been confirmed, the first step is to completely off-load and immobilise the foot to protect the bones and prevent further collapse. We have a range of boots and braces to help with this, and you may need to use crutches during this time. You will be carefully monitored throughout this time so you know when it’s safe to transition out of your boot or walker.
After your bones have healed, custom foot orthotics, good supportive footwear, and even braces may be needed to help you resume daily activities comfortably while helping prevent the condition from recurring. It is important to note that many people are left with significant changes in their foot structure which can increase their risk of ulcers and other complications. This is where your orthotics will be designed to help accommodate these changes and support your foot health. You may also need to make some modifications to your physical activities for some time, which your podiatrist will advise you on.
In many cases, we work closely with your doctor to provide the best outcomes for your feet and address all of your individual needs. In some cases, surgery may be indicated.
FAQs
Is Charcot Foot a common condition?
Charcot Foot is relatively rare compared to other foot conditions, though we definitely see it in our clinic. It is most commonly associated with underlying neuropathy, often seen in individuals with diabetes.
Can Charcot Foot affect both feet?
Yes, Charcot Foot can affect both feet, although it typically begins on one foot. The condition may progress to involve the other foot if left untreated or if both feet are subjected to similar stress or trauma.
What are the treatment options for Charcot Foot?
The primary goal of treatment for Charcot Foot is to stabilise the foot, promote healing, and prevent deformity and further complications. This often involves immobilisation, offloading the affected foot with casts or special footwear, and reducing weight-bearing activities. Please see our management options above for more information. In some cases, surgical intervention may be necessary to correct deformities or address complications.
How long does it take for Charcot Foot to heal?
The healing time for Charcot Foot can vary depending on the severity of the condition, a person’s overall health, and the chosen treatment approach. It typically takes several months for the acute phase to subside, and the complete healing process may continue over a period of one to two years.
Can Charcot Foot lead to foot deformities?
Yes, Charcot Foot can lead to foot deformities if not properly managed – and often does. The weakened bones and ligaments associated with Charcot Foot can result in structural changes and collapse of the foot arches, leading to deformities such as rocker-bottom foot, bony prominences, and foot ulcers.
What are the long-term complications of Charcot Foot?
If left untreated or not managed effectively, Charcot Foot can lead to several long-term complications such as foot deformities, chronic ulcers, infections, joint instability, limitations in mobility, and an increased risk of fractures. Proper treatment and ongoing care are crucial to minimise these complications.
Can Charcot Foot recur after treatment?
While recurrence of Charcot Foot after successful treatment is uncommon, it is essential to continue managing the underlying condition, such as diabetes or neuropathy, to minimise the risk. Following a comprehensive treatment plan, regular foot examinations, and adopting preventive measures can help reduce the chances of recurrence.
Can Charcot Foot be prevented?
Although it may not be possible to prevent Charcot Foot entirely, managing underlying conditions, such as diabetes or neuropathy, can reduce the risk. Proper foot care, including regular foot inspections, maintaining good blood sugar control, wearing appropriate footwear, and seeking prompt medical attention for any foot injuries, can help prevent complications.
Can Charcot Foot lead to amputation?
In severe cases or if left untreated, Charcot Foot can lead to complications that may necessitate amputation. This is something that should be discussed with your doctor or orthopaedic surgeon. However, with early diagnosis, appropriate treatment, and ongoing care, the risk of amputation can be significantly reduced. Close monitoring by a podiatrist and adherence to recommended treatment plans are crucial in preventing such outcomes.

