Do your feet seem to sweat more than others? Do they regularly carry an unpleasant…
Why do high blood sugar levels result in a greater risk for peripheral arterial disease & what can you do to reduce your risk?
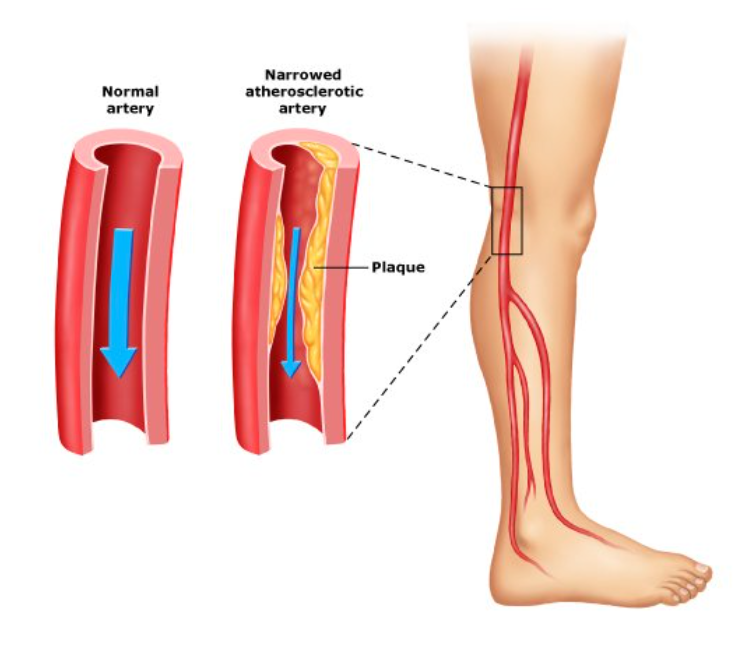
Peripheral arterial disease (PAD) is a condition in which your arteries, or large blood vessels, become narrowed and can’t carry as much blood to the outer parts of your body, such as your feet and legs, which can increase your risk of wounds, ulcers, and in some rare cases, amputations. There are many risk factors for developing PAD including high cholesterol, high blood pressure, smoking, obesity, and high blood sugar levels and diabetes.
Here we’ll delve into how high blood sugar levels can put you at greater risk of developing PAD, what you can do to reduce your risk, and why working alongside a podiatrist is recommended to reduce your chance of complications while maintaining your overall foot and leg health.
Why Do High Blood Sugar Levels Result In A Greater Risk For Peripheral Arterial Disease?
 Biologically speaking, our blood vessels are lined by specialised cells called endothelial cells which maintain the structure of the blood vessels and support them to function well. In healthy individuals, these endothelial cells produce a chemical called nitric oxide (NO). NO helps our blood vessels and arteries to relax and widen, and prevents them from becoming damaged by inflammation or clots.
Biologically speaking, our blood vessels are lined by specialised cells called endothelial cells which maintain the structure of the blood vessels and support them to function well. In healthy individuals, these endothelial cells produce a chemical called nitric oxide (NO). NO helps our blood vessels and arteries to relax and widen, and prevents them from becoming damaged by inflammation or clots.
However, in patients with high blood sugar levels or diabetes, this constant increase in blood sugar levels can cause endothelial cells to produce low levels of NO, causing the arteries to constrict, or become narrower, which allows more inflammation and clotting to take place. Because of this, the wall of the artery gets damaged over time, and a fatty streak called plaque builds up along the lining of the arterial walls. Ultimately, this plaque can block the artery and reduce the blood flow that can travel to your legs and feet, meaning that your tissues in your legs and feet are deprived of oxygen, and are more likely to develop ulcers and struggle to recover from wounds.
How Do I Know If I Have Peripheral Arterial Disease?
The most common symptoms of PAD are pain, cramping or aching in the calves, thighs or buttocks which gets worse with physical activity, but nearly 50% of all patients with PAD are actually asymptomatic. This may be because diabetic patients often have damaged nerves, known as peripheral neuropathy, meaning that they are unable to detect pain accurately. Other signs and symptoms include:
- Coldness in your legs and feet
- Change in colour of your legs, feet and toes
- Hair loss on your feet or legs
- Shiny skin on the legs
- Night cramps
- Leg weakness or fatigue when walking
- Slow toenail growth
- Wounds or sores on your toes or feet that don’t heal well
If you have noticed any of the above signs or symptoms, we recommend booking an appointment with an experienced podiatrist who can perform a diabetes foot screening, assess your medical history, check for risk factors, make your vascular, neurological, biomechanical, dermatological and footwear assessments and create a targeted a management plan.
It’s often hard to detect symptoms of PAD, especially in the initial stages. Regular checkups can help with early diagnosis and treatment that can keep the worst symptoms and complications of PAD at bay.
What Can You Do To Reduce Your Risk?
Healthy lifestyle choices are the first step to help to prevent PAD:
- Smoking: The most important step you can take is to stop smoking, or don’t start in the first place
- Regular exercise: Aim to do some form of movement that you enjoy for 30 minutes on most days of the week
- Healthy eating: Manage your blood sugar levels, cholesterol and weight by eating a healthy diet high in fibre and across a range of food groups
- Stress control: Implement ways to keep your stress levels down, this might mean changing aspects of your life, or using exercises such as meditation or yoga, and time with friends and family
- Manage other conditions: Seek support to treat and help to prevent conditions that can raise your risk of developing PAD such as high blood pressure, diabetes, and high cholesterol.
- Work alongside a podiatrist: For those who struggle with high blood sugar or diabetes, it’s now recommended that all of these patients be supported by podiatrists, who can reduce your risk of foot deformities and health complications, including amputations by more than 50%, through regular foot examinations, identifying biomechanical faults, regularly treating calluses, prescribing supportive braces and orthotics, and even, recommending appropriate footwear. To read more about diabetic footwear, check out this blog article.
If you’re concerned about peripheral arterial disease, our experienced podiatrists are here to help, with a comprehensive examination and a targeted treatment plan to prevent the impacts that PAD can have on your feet and legs. To book an appointment with one of our friendly podiatrists, contact us here.
